Right L3-L4 Foraminal Lumbar Disc Herniation Approached From the Contralateral Side Through an “Over the Top” Minimally Invasive Laminectomy
M.A. Roldán Serrano, MD
Raj Nangunoori, MD; Roger Härtl, MD
Weill Cornell Brain and Spine Center. New York, NY (USA).
History & Examination
The patient was a 55-year-old female referred evaluation with a chief complaint of right leg pain radiating across the anterior thigh to the medial knee in an L3 distribution after several weeks of failed conservative therapies. Upon evaluation, the patient did not have any mechanical back pain. According to the patient, the pain was severely limiting her professional life and recreational activities due to her symptoms.
Examination
The patient was neurologically intact except for trace weakness in right knee extension. Pain/paresthesias in an L3 dermatome on the right.
Imaging
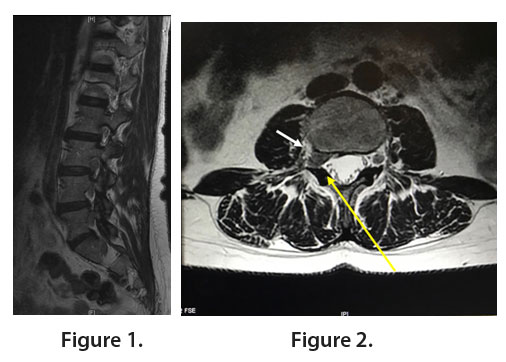
MRI T2-weighted sagittal (Figure 1) and axial view (Figure 2, white arrow) of the patient’s lumbar spine demonstrated a right-sided soft L3-4 disc herniation causing compression of the exiting right L3 nerve root at the entrance to the neural foramen. The yellow arrow indicates the approximate trajectory to access the disc herniation using the proposed approach.
Diagnosis
Right L3 radiculopathy due to L3-L4 right foraminal lumbar disc herniation via 18 mm-tubular retractor.
Treatment
Goal: Decompression of the right L3 nerve root and removal of the herniated disc
Challenge: Access to the foraminal disc herniation without causing instability.
Surgical Plan: Contralateral “over the top” minimally invasive laminectomy at L3-4 from a left-sided approach.
Surgical Procedure: Due to the anatomical location of the disc, a standard paramedian approach would require significant drilling of the facet joint and the potential for creating iatrogenic instability. An “outside-in” (aka extraforaminal) approach, as is used for a far-lateral disc herniation would be less effective in this scenario as the disc herniation is purely intraforaminal in nature. Due to the progressively smaller diameter of the spinal canal at rostral lumbar levels, a contralateral approach and laminectomy allows for retraction of the thecal sac to access the disc herniation and decompress the exiting nerve.
Figure 3 demonstrates the intraoperative view through the tubular retractor demonstrating the spinolaminar junction, which is the optimal starting point for drilling to expose the ipsilateral ligamentum flavum. Once the ipsilateral laminotomy is complete, the insertion of the ligament is identified and dissected away from the underlying dura (Figure 4). The midline epidural fat is also visualized at this stage.
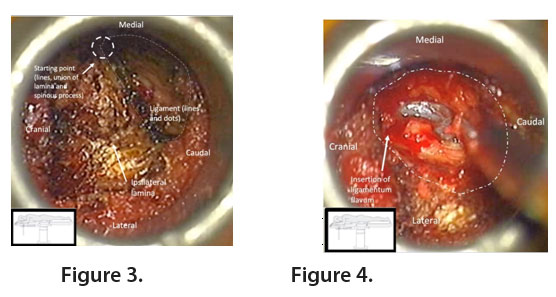
Figure 5 shows the view of the base of the spinous process and contralateral hemilamina after tilting of the tube and patient away from the surgeon. A contralateral laminotomy (lines and dots) is performed over the contralateral yellow ligament moving the drill in the direction of the arrows. The contralateral ligament is removed exposing the lateral recess of the opposite side, demonstrating the exiting right L3 nerve as well as a disc bulge (dots).
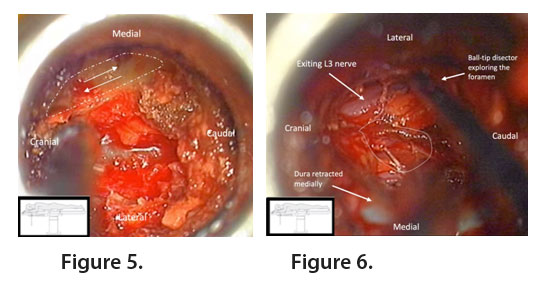
Gentle pressure with the ball-tip dissector allows for slow extrusion of the herniated disc (Figure 7). A bayoneted knife is then used to remove additional disc material (Figure 8).
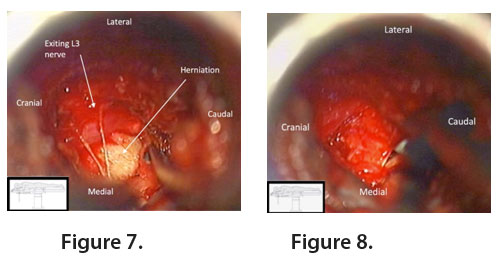
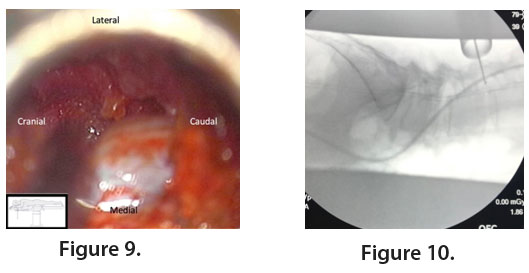
Figure 9 demonstrates the final view once decompression and discectomy is complete. A final fluoroscopy image (Figure 10) was taken to demonstrate decompression of the right-sided L3-4 neural foramen.
Outcome
Postoperatively, the patient did well and remained in the hospital one night and was discharged on postoperative day 1 with resolution of her preoperative leg pain.
Discussion
Currently, tubular retractors are commonly used for minimally invasive procedures in the lumbar spine. The advantages of minimally invasive surgery are well documented in the literature due to preservation rather than destruction of soft tissue structures.
For foraminal and extraforaminal herniations, the far-lateral (an “outside-in”) approach has also been described. However, this approach is challenging due to the unfamiliar anatomy compared with a standard paramedian approach for a minimally invasive microdiscectomy. The far lateral approach is also most advantageous in cases where there is a true extraforaminal disc herniation. In the illustrated case, the disc herniation was located at the entry to the neural foramen, which if using conventional techniques can only be reached by removal of a significant portion of the facet joint. furthermore, if a far lateral approach was used, a significant amount of lateral facet and lateral pars would need to be removed to gain access to disc herniation in the neural foramen. In contrast, an “over-the-top” laminectomy allows for access to the contralateral exiting nerve, foramen and disc with minimal disruption of the facet joints. Care must be taken to avoid inadvertently drill the pars on the ipsilateral side due to the progressively decreasing diameter of the spinal canal at rostral lumbar levels.
References:
- M Alimi, CP Hofstetter, JM Torres-Campa, R Navarro-Ramirez, GT Cong, I Njoku, R Härtl. Unilateral tubular approach for bilateral laminotomy: effect on ipsilateral and contralateral buttock and leg pain. Eur Spine J. 2017; 26(2):389-396.
- C Wipplinger, C Melcher, RN Hernandez, S Lener, R Navarro-Ramirez, S Kirnaz, FA Schmidt, E Kim, R Härtl. “One and a half” minimally invasive transforaminal lumbar interbody fusion: single level transforaminal lumbar interbody fusion with adjacent segment unilateral laminotomy for bilateral decompression for spondylolisthesis with bisegmental stenosis. J Spine Surg. 2018; 4(4):780-786.